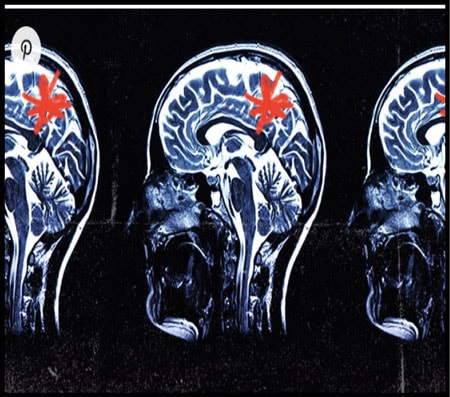
Evidence suggests that microglia—the primary immune cells in the brain—may directly contribute to the development of neurodegenerative conditions such as Alzheimer’s disease (AD).
Due to technical challenges, scientists have not been able to decipher the molecular mechanisms underlying microglia activity or function in healthy and diseased brains.
Scientists have now developed a new method based on the gene-editing tool CRISPR to identify genes that modulate the function of microglia.
By identifying the genes involved in disease-driving states of microglial activity, scientists were able to switch the genes on and off, paving the path for developing new therapies for AD.
In a recent study published inNature NeuroscienceTrusted Source, scientists revealed a novel screening platform for characterizing genes that regulate specific microglialTrusted Source functions which may contribute to Alzheimer’s disease (AD).
Characterizing regulatory genes that cause microglia to switch from a healthy state to a diseased state, such as in the brains of individuals with AD and other neurodegenerative conditions, could help develop therapeutics that target these genes or the proteins encoded by these genes.
“Since microglia are guardians of the brain’s homeostasis, it is important to identify specific drivers that lead to neuronal toxicity for therapeutic intervention. Our new CRISPR screening platform […] enables us to identify these drivers in a rapid, scalable manner. We already uncovered druggable targets that control microglia states, and the next steps would be to test these in relevant preclinical models.”
— Dr. Li Gan, study co-author and neuroscientist at the Weill Cornell Medical College, speaking to Medical News Today The role of microglia AD is the most common form of dementia, accounting for 60-80% of all dementia cases. Despite the advances in the understanding of AD, there is a lack of effective treatments for this neurodegenerative disease.
The accumulation of the misfolded beta-amyloidTrusted Source protein into clumps or plaques is one of the hallmarks of AD. A considerable amount of research has focused on mutations that lead to the abnormal processing of the beta-amyloid protein and, subsequently, its accumulation.
However, treatments targeting the pathways involved in the processing of beta-amyloid have not been successful.