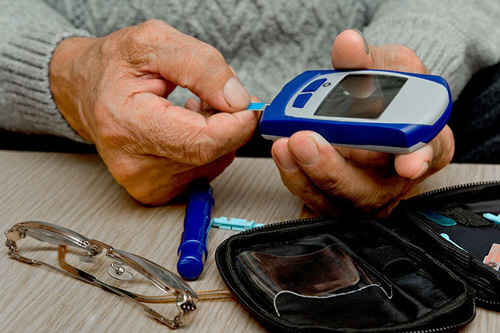
A study has revealed how poor management of blood glucose levels in people with type 1 diabetes can increase their risk of complications decades later.
In 2016, around 1.3 million adults in the United States, about 0.55% of the adult population, had type 1 diabetes, according to the Centers for Disease Control and Prevention (CDC).
As a result, people with the condition are unable to generate enough insulin to regulate the amount of glucose, or sugar, circulating in their blood.
Over time, high levels of blood glucose, an issue called hyperglycemia, can damage tissues all over the body, including in the eyes, kidneys, nervous system, and cardiovascular system.
Even if a person regulates their blood glucose later in life, early episodes of poor glycemic control can have permanent effects. The scientists profiled a type of epigenetic modification called methylation in DNA from cells in archived blood samples. Methylation switches off genes, preventing them from producing the proteins that they encode.
The blood samples were collected some 2 decades earlier, from patients with diabetes who were closely monitored as part of the Diabetes Control and Complications Trial (DCCT). This study showed that people who kept their blood glucose levels close to the normal range had significantly fewer diabetic complications during the 10 years of the study.
The researchers behind the current investigation analyzed the DNA in samples from 499 randomly selected DCCT participants who had been subsequently included in a follow-up study, called Epidemiology of Diabetes Interventions and Complications.
SICKLE CELL DISEASE: CANNABIS MAY IMPROVE PAIN-RELATED MOOD: A new study has found that cannabis may improve the mood of people who experience chronic pain from sickle cell disease.
New research suggests that cannabis may help improve the mood of people with chronic pain from sickle cell disease. This proof of principle study also found that cannabis was a relatively safe intervention. The research paves the way for future studies to verify the initial findings and expand the investigation on cannabis-based interventions on chronic pain.
According to the Centers for Disease Control and Prevention (CDC), sickle cell disease is a type of red blood cell disorder that causes the cells to become misshapen and look similar to the crescent shape of a sickle.